Health Care Workforce Shortages: An Updated Look
Last week, the Senate Committee on Health, Education, Labor and Pensions held a hearing titled “Examining Health Care Workforce Shortages: Where Do We Go From Here?”
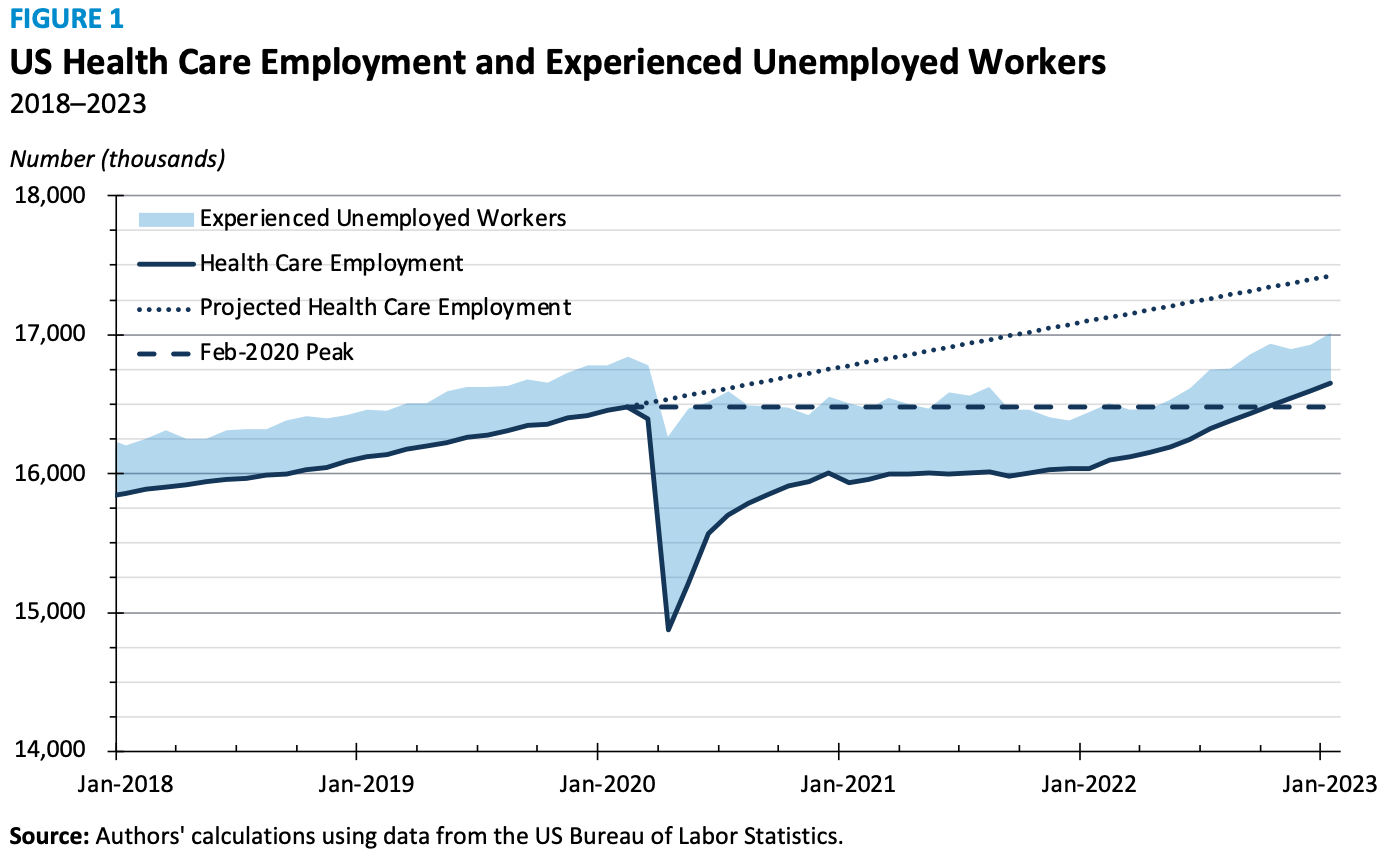
When we first wrote about this issue seven months ago, health care employment was 175,600 below its February 2020 peak and 954,000 below where it would have been had it continued to grow at its pre-pandemic rate. Now, health care employment has increased to 16.6 million (a new high), but there is still a large gap compared to pre-pandemic projections. As of January 2023, health care employment is 767,000 below the trend, a 4.4 percent shortfall.
Job openings in the sector remain at historic levels – 1.9 million in December 2022 – compared to an average of 1.6 million in 2021 and 1.1 million in 2019 and 2020. Figure 1 shows US health care employment relative to the pre-pandemic trend, as well as the number of experienced unemployed workers – those individuals available and actively looking for work who were previously employed in the health care sector. The number of experienced unemployed has declined to 359,000, which is approximately the same as two years before the pandemic and slightly less than half of the current projected employment gap.
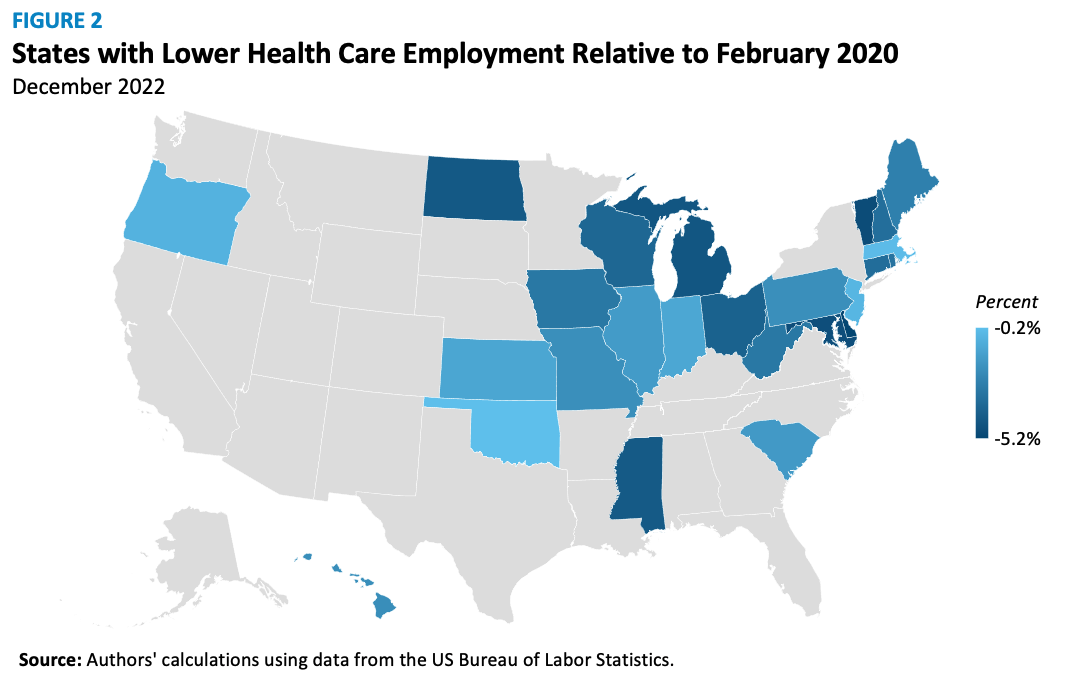
Half of the states, including all in New England and most in the Midwest, have health care employment lower than in February 2020 (see Figure 2). The other states, including the four most populous – California, Texas, Florida, and New York – have reached or surpassed their February 2020 health care employment levels as of December 2022, the latest state-level data.
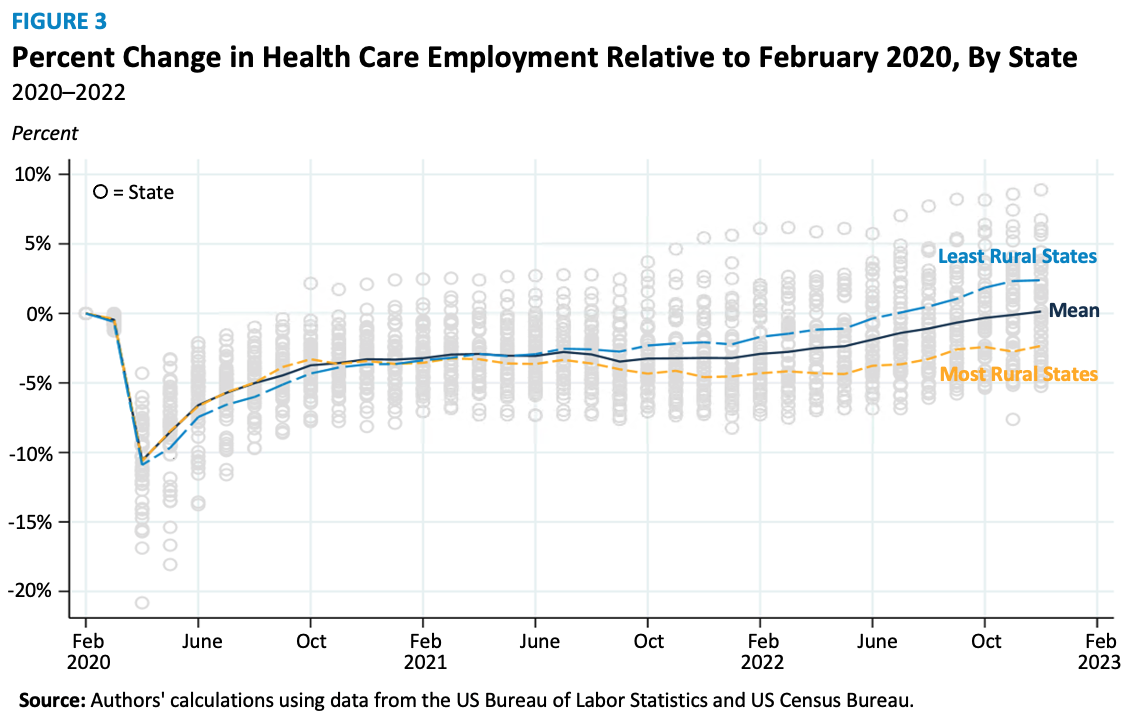
The slower rates of employment recovery are especially noticeable in states with higher percentages of their population in rural areas, as seen in Figure 3. The five most rural states (Vermont, Maine, West Virginia, Mississippi, and Montana), with rural populations at or above 46 percent, are, on average, 2.3 percent below their February 2020 levels. Conversely, the five least rural states (District of Columbia, California, Nevada, New Jersey, and Florida) are, on average, 2.3 percent above their February 2020 levels. Generally, a 1 percentage point increase in a state’s rural population is associated with a 0.7 percentage point larger gap in health care employment since January 2021.
This workforce shortage problem is easy to observe, but solutions are harder to come by. Broadly speaking, solutions generally fall in two camps: increasing supply or decreasing demand.
Increasing the supply of health care professionals quickly is challenging due to the education and training required. Becoming a physician, for example, can take up to 10 years. Other health care professionals must attend college or graduate school and pass licensing exams. And regarding potential nurses, Dean Sarah L. Szanton of Johns Hopkins University School of Nursing has testified that “about 90,000 qualified applications are turned down from nursing schools each year due to lack of space. . .The nursing shortage is, in large part, a nurse faculty shortage.”
Decreasing the demand for health care professionals is difficult as well. A healthier population would help but may not be feasible, and demographic trends like the aging population make this solution even less likely. Changes to health care delivery and scope of practice regulations could reduce the demand for labor in some settings. Health care technology, for example, can allow professionals to serve patients more efficiently, and permitting nurses to perform some tasks normally reserved for physicians could also alleviate physician demand.
So, where do we go from here? Nowhere fast, we suspect. In the short term, efforts should concentrate on those areas still facing job shortages, particularly large rural areas. State-level policy changes, as opposed to federal policy levers may be more efficient, given the disparate geographic impact of the shortage.
This article first appeared on February 21, 2023 at AEIdeas. AEIdeas is a publication of the American Enterprise Institute (AEI).